The birth of a child brings immense joy, but also concerns about their health and well-being. For parents who have experienced the challenges of hypospadias in their firstborn, questions about the risk of recurrence in a second child understandably arise. This blog aims to provide insights and guidance on this sensitive topic.
What is Hypospadias and is it necessary to repair it?
Hypospadias is a birth defect affecting boys, characterized by an abnormally positioned urethral opening. This opening, which normally lies at the tip of the penis, can be located anywhere along the shaft, scrotum, or even perineum. While the severity varies, hypospadias can affect urination, sexual function, and self-esteem. For very minor hypospadias without any chordee, family may choose to not do surgery but after consultation with an expert hypospadias surgeon. For all other hypospadias, correction surgery is recommended.
Is My Second Child at Risk of Hypospadias?
The possibility of hypospadias occurring in a second child depends on several factors:
- Family history: If the father or a brother has hypospadias, the risk in subsequent sons increases. Estimates suggest 5-6% risk for a second son and this risk increases further if both father and brother are affected.
- Environmental factors: Exposure to certain environmental toxins, such as pesticides and herbicides, may play a role. These pesticides are known to be endocrine disruptors, they interfere with the androgen and oestrogen signalling pathways during genital development, hence causing hypospadias. This is a hypothesis, and studies are still under process to clearly link exposure of pesticides to occurrence of hypospadias. There have been studies showing higher risk of hypospadias due to plasticisers in the single use plastic bottles. The chemicals here act as male hormone blockers and interrupt development of penis, hence causing hypospadias.
- Hormonal exposure in pregnancy: During pregnancy, certain hormones may be advised for the mother to decrease the chance of preterm labour or miscarriage. This is common after invitro fertilization (IVF) conception, twin pregnancy and in precious pregnancies. Carmichael in his study reported that the use of progesterone to prevent early pregnancy loss was associated with risk of developing moderate to severe hypospadias1.
- Maternal health: Maternal smoking, pre pregnancy obesity, folic acid deficiency is some of the associated factors causing hypospadias.
Understanding the Probabilities of second child with hypospadias
While the above factors influence the risk, it’s important to understand that they do not guarantee the condition’s recurrence. Each pregnancy is unique, and predicting with certainty is impossible.
Here’s a breakdown of the estimated risks:
- For a family with no history of hypospadias, the general risk is around 1 in 250 births
- If the father has hypospadias, the risk rises to about 1 in 50
- With a brother affected, the risk increases to approximately 1 in 30
- When both father and brother are affected, the risk becomes roughly 1 in 20
Moving Forward: Taking Charge
Despite the uncertainty, proactive measures can empower parents to understand hypospadias and get proper counselling to understand the possibility of hypospadias in their second child. This includes:
- Genetic counselling: Consulting a genetic counsellor can provide personalized risk assessment and guidance based on your specific family history. Genetic analysis can help us know the possibility of hypospadias in subsequent pregnancies.
- Preconception care: Maintaining good health and avoiding harmful substances during pregnancy can minimize potential environmental influences. Folic acid supplementation should be started before conception and continued during the first trimester to avoid hypospadias.
- Prenatal testing: While currently no specific tests diagnose hypospadias in utero, advanced ultrasound technology may detect anatomical abnormalities suggestive of the condition. This is possible only in countries where predetermination of sex of the child is allowed in ultrasound in pregnancy.
- Early diagnosis and intervention: If hypospadias is diagnosed after birth, early intervention through specialized treatment can optimize outcomes. Early referral to an expert hypospadias surgeon, early surgery can help the parents and child to overcome the hypospadias problem.
Remember that Knowledge is power. By understanding the risk factors and available resources, parents can navigate the uncertainty surrounding hypospadias and make informed decisions about their second pregnancy.
Let’s work together to raise awareness and offer support to families affected by hypospadias.
Additional Resources:
- Carmichael SL, Shaw GM, Laurent C, Croughan MS, Olney RS, Lammer EJ. Maternal Progestin Intake and Risk of Hypospadias. Arch Pediatr Adolesc Med.2005;159(10):957–962. doi:10.1001/archpedi.159.10.957
- Urology Care Foundation: https://www.urologyhealth.org/educational-resources/hypospadias
- National Institute of Child Health & Human Development: https://pubmed.ncbi.nlm.nih.gov/35398463/
- Hypospadias Association: https://heainfo.org/
About Hypospadias Foundation
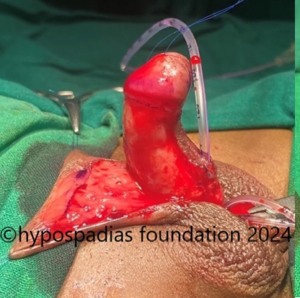
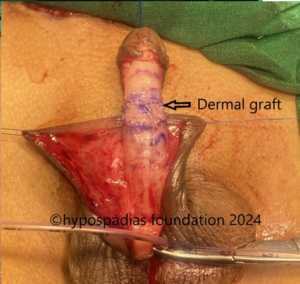
Hypospadias Foundation is a centre specialized for treatment of children with hypospadias. Our expertise in hypospadias makes us one of the best centres for hypospadias repair in the world. We treat children from more than 25 countries in the world and from all over India. Our dedication in this field has helped us achieve excellent outcomes. Hypospadias foundation is located at MITR Hospital in Kharghar, Navi Mumbai in the state of Maharashtra.
Dr A K Singal is an expert and top hypospadias surgeon in India. He is a gifted surgeon and his expertise in this area has helped us achieve excellent outcomes in primary and failed hypospadias in children as well as adults.
Dr Ashwitha Shenoy is an expert hypospadias surgeon with special interest in hypospadias and pediatric urology. Both Dr Singal and Dr Shenoy work together to give best results for hypospadias surgery in India for both children and adults.
Contact Form for Hypospadias Foundation
Please fill all clinical details and upload pictures and clinical summaries (if available)