Hypospadias and small penis size: diagnosis and treatment
Hypospadias is a congenital malformation affecting about 1 in 250 male births, this amounts to more than 50,000 children born in India every year with hypospadias.in this condition, the urethral opening lies on the underside of the penis instead of its tip. While severity varies, hypospadias is sometimes associated with small penile size. Let’s delve into the facts about hypospadias, its effect on size and treatment options.

Understanding Hypospadias:
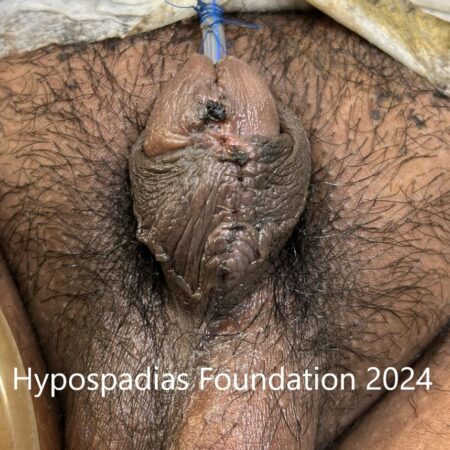
During development of penis between 8-12 weeks of pregnancy, the urethra (urinary pipe) starts forming from the base of the scrotum to penis, finally proceeding forwards towards the tip. Hypospadias occurs when the tissue forming the urethra doesn’t fully close during fetal development. This results in the urethral opening appearing anywhere on the underside of the penis, from the glans (mildest form) to the scrotum (severest form).
Hypospadias and Penile Size:
The relationship between isolated hypospadias and penile size is complex. Studies show the following:
- No significant difference in length: Research suggests that overall penile length in infants and prepubescent boys with isolated distal or minor hypospadias is comparable to unaffected boys in most boys. While the penis may be small in proximal or severe hypospadias.
- Chordee causes the penis to look small: Hypospadias can cause the penis to curve downwards, a condition called chordee.This can make the penis appear shorter.
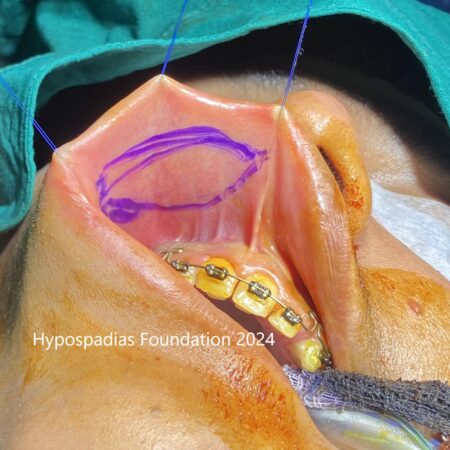
- Surgical considerations: Reconstructive surgery for hypospadias aims to correct the urethral opening’s position and straighten the penis. While some techniques may involve using tissue flaps, these typically don’t significantly impact penile length.
Some people with hypospadias may have an actual short penis size. For this to be understood, lets first understand how hormones work to lead to penis growth:
Penis formation is complete by 12 weeks of pregnancy. During the rest of the pregnancy, under the influence of hCG hormone, which is released from placenta of the mother, the testes of developing baby produce a hormone called testosterone. Testosterone is the main male hormone, which is responsible for male pattern of facial hair growth, beard formation, muscle development, thickening of voice etc. which are male external features at puberty. However, testosterone is the not main hormone responsible for penis growth. Testosterone gets converted into dihydrotestosterone (DHT) which is much stronger variant of testosterone and is the main hormone responsible for penis size increase. Collectively, testosterone and dihydrotestosterone are called androgen hormones. Both testosterone and dihydrotestosterone act via androgen hormone receptors. For a moment think of a lock and key mechanism. Hormones are the keys which go and bind to receptors which are the locks. Working together, the lock and key, lead to penis development. So, inadequate androgen action either due to
- Less production of testosterone
- Testosterone not getting converted to dihydrotestosterone.
- or receptors are not working,
Then the penis size will remain small.
Hormonal Reasons which may cause short penis length in hypospadias:
- Hormonal disorders: Some children with hypospadias may have hormonal issues like testosterone production defect, androgen insensitivity or 5 alpha reductase deficiency. Whenever we find penis size to be very small along with hypospadias, we typically do a detailed hormonal evaluation to find out the real cause and then treat it.
- Low birth weight or premature babies: Our experience shows that babies which are born ahead of their full-term date of birth usually have a smaller penis. This happens as the main penile growth in a baby in pregnancy happens in the last few weeks. If the baby does not receive hCG in the last weeks of pregnancy, then testosterone and DHT is also low, leading to smaller size of penis. Same thing happens in babies who have IUGR or low birth weight, their body produces smaller quantities of hormones for penile growth in the last few weeks of pregnancy.
Addressing small size of penis with hypospadias:
First, penile size should be measured in all children with hypospadias. Two measurements are important – penile length (stretched penile length) and glans diameter. Normally in a 6-month-old child, the SPL should be atleast 35mm and glans diameter should be atleast 14 mm.
If the child was born preterm or was low birth weight, and the glans diameter is atleast 11-12 mm, then as a first choice we give testosterone injections. These injections are given 1 month apart in 2 doses. Typically, it takes 3 months for the penis size to become normal. And then we plan the hypospadias repair surgery. Testosterone injection response also tells us how the penis will respond to natural testosterone at time of puberty and is a good marker to assure the parents and the doctor.
If the penile size is very small in a full-term baby or the baby has severe hypospadias, then we do a full hormonal test battery consisting of LH, FSH, AMH, Testosterone and then give 3 doses of hCG hormone to stimulate the testis. Post hCG stimulation, we test for testosterone and dihydrotestosterone again. There are three possibilities at this stage:
- Testosterone does not rise: That means there is testosterone biosynthetic defect. This can be solved by giving external testosterone injections.
- Testosterone rises normally but DHT does not rise as evidenced by T/DHT ratio: This is suggestive of 5 alpha reductase enzyme defects. Such children will require DHT gel to help them achieve normal penile size.
- Both Testosterone and DHT rise normally: There is a possibility of androgen insensitivity in such cases. We give testosterone injections, but they may not work in all the cases.
All these tests and their interpretation should be done by an experienced pediatric urologist or a hypospadias surgeon or a pediatric endocrinologist.
Summary:
At Hypospadias foundation India, we have been taking care of children and adults with hypospadias for last 15 years with best-in-class results. Children with hypospadias and small penis should be well evaluated whenever needed by a hypospadias expert. This evaluation is important in childhood itself to lay a future healthy path for the child. There is detailed measurement and counselling done before any hypospadias surgery at our centre. Dr A.K.Singal is currently rated as the best hypospadias surgeon expert in India for such cases. Dr Singal works along with Dr Ashwitha Shenoy in MITR Hospital Navi Mumbai to help children and adults get good results for treatment of hypospadias. If you need a second opinion for hypospadias, please do write to us at hypospadiasfoundationindia@gmail.com or fill up this contact form.
References:
- American Urological Association: https://www.hypospadias-society.org/
- National Institutes of Health: https://www.ncbi.nlm.nih.gov/books/NBK564407/
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/hypospadias/symptoms-causes/syc-20355148
Contact Form for Hypospadias Foundation
Please fill all clinical details and upload pictures and clinical summaries (if available)