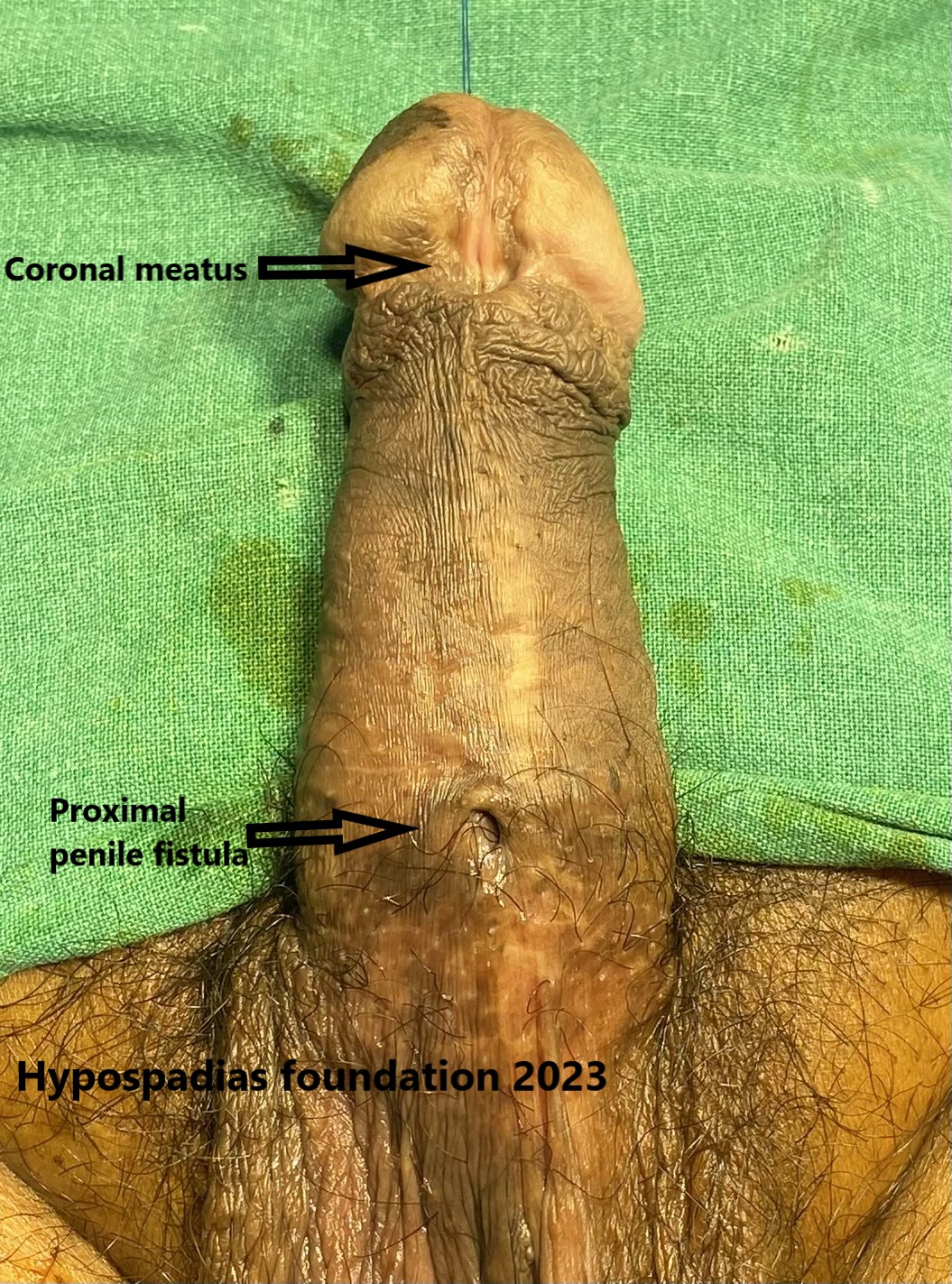
Hypospadias is a birth defect that affects 1 in 150 male babies. It occurs when the urethra, the tube that carries urine out of the body, doesn’t develop properly. Instead of opening at the tip of the penis, the opening is somewhere on the underside of the penis. In some cases, hypospadias may be associated with underlying hormonal issues that can affect the growth of the penis. While the exact cause remains unknown, some theories link it to abnormal hormonal development during pregnancy. In these cases, hormonal testing might be recommended before surgery to assess potential underlying conditions.
Hormonal Influences:
- Testosterone: This male sex hormone plays a vital role in the development of the penis and scrotum. Low fetal testosterone levels might be a contributing factor to small penile size in some hypospadias cases.
- Dihydrotestosterone (DHT): Testosterone is converted to DHT by an enzyme 5 alpha reductase. DHT is crucial for the formation of the urethra along the underside of the penis. An imbalance in DHT levels could potentially influence hypospadias development and associated small penile size.
At hypospadias foundation, we do the preoperative measurement of the size of the penis of all children with hypospadias. We check two parameters i.e Stretched penile length (SPL) and Glans diameter (GD).
The protocol which we follow at our centre is as follows:
| 1. | SPL <30mm | GD<12mm | Hormonal testing |
| 2. | SPL<30mm | GD 12-14mm | Two doses of testosterone before surgery |
| 3. | SPL>30mm | GD>14mm | Normal |
When are Hormonal Tests Performed?
While not routine for all hypospadias cases, hormonal testing should be done in these situations:
- Small phallus: The presence of a small phallus alongside hypospadias might indicate hormonal imbalances. If the size of the penis, SPL< 30mm and GD< 12mm then hormonal testing is mandatory
- Severe Hypospadias: If the hypospadias is severe, affecting other genital structures or accompanied by undescended testicles (cryptorchidism), hormonal tests along with karyotyping might be recommended to diagnose a case of DSD (disorder of sexual differentiation)
- Family History: A family history of hypospadias or other genital malformations could also warrant hormonal testing.
Which are the hormonal tests recommended in case of hypospadias?
hCG stimulation test is the hormonal test recommended in cases of hypospadias. On day 1, blood sample is collected and first dose of Inj hCG is administered. On day 2 and day 3, Inj hCG is administered. On day 4, serum testosterone and 5-alpha Dihydrotestosterone levels are measured. The dose of hCG is 3000IU/m2 BSA. In this test pre hCG injection hormone (testosterone) levels are compared with post hcg injection hormone (testosterone and DHT) levels.
This test is interpreted as follows:
- There should be a rise in testosterone levels after hCG injection (more than 2 times rise after hCG injection)
- There should be conversion of testosterone(T) to dihydrotestosterone (DHT). The normal ratio of T/DHT is under 8 and is considered abnormal above 16. Between 8-16 is considered borderline.
If the hCG stimulation test shows normal rise in testosterone and normal T/DHT ratio, then the child is given two doses of testosterone in the preoperative period. This should effectively normalize the size of the penis for that age.
If the hcg stimulation tests shows increase in the levels of testosterone but inadequate conversion to DHT, then it implies that there may be 5 alpha reductase enzyme deficiency. These children do not have sufficient DHT in their body hence they will need DHT supplementation of to improve the size of the penis.
If the hCG stimulation test results are borderline, then we prefer to give two doses of Injection testosterone and assess the response. The ones who do not respond to testosterone may need DHT gel supplementation.
Rarely testosterone and DHT may not increase the size of the penis. The cause for this may be androgen insensitivity. In androgen insensitivity, the body’s cells are unable to respond to androgens, male hormones.
Hormonal analysis in hypospadias is important because it indirectly predicts the child’s future. If the hormone levels are normal, then there will be natural growth of the penis at puberty. If the hormone levels are abnormal then the child may need hormonal supplementation at puberty. But this decision is taken at puberty if the natural growth is inadequate.
Importance of Consulting a Pediatric Urologist:
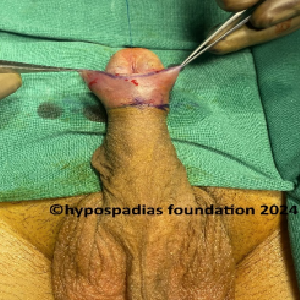
If your child requires hypospadias surgery, a pediatric urologist will determine if hormonal testing is necessary based on the specific condition and individual factors. They will explain the rationale behind the tests and address any concerns you may have. Surgical results in a small penis are suboptimal with higher risk of complications.
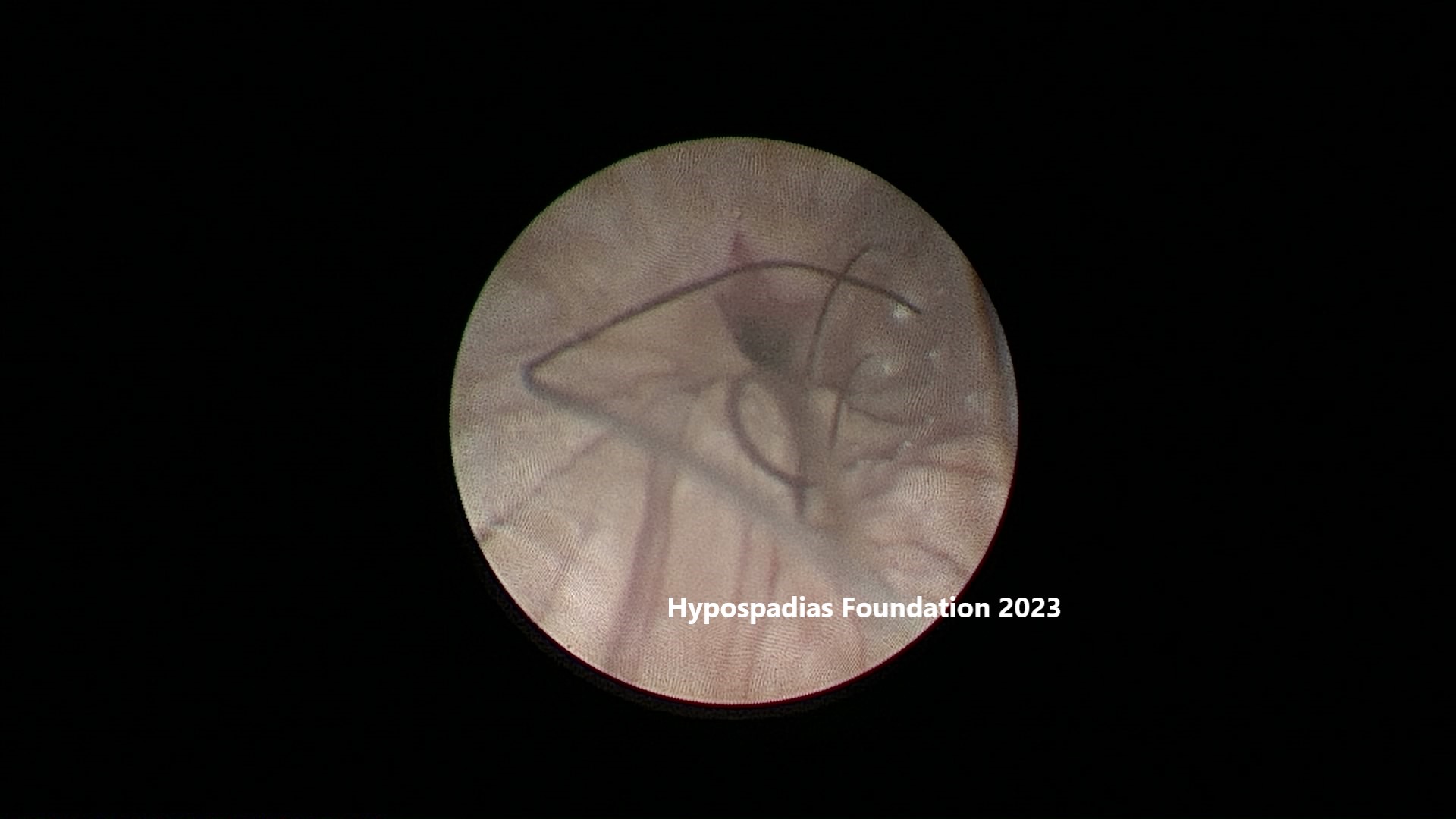
At hypospadias foundation, we believe in complete care when it comes to hypospadias. Penile measurements in the OPD, preoperative hormone tests and supplementation if required and planning of surgery, every step is important to achieve our goal of successful hypospadias surgery with no complications. Dr Singal and Dr Shenoy are the best hypospadias surgeons for these reasons. Every child is assessed thoroughly and taken utmost care to yield excellent results.
Dr A K Singal is a highly experienced surgeon and is regarded as the best hypospadias surgeon in India and in the world for treating children and adults with hypospadias. If you are looking for a highly skilled and experienced pediatric urologist and hypospadias surgeon for yourself or your child, then Dr Singal is an excellent choice.
Dr Ashwitha Shenoy is an expert pediatric surgeon with a special interest in pediatric urology and hypospadias. Dr Singal and Dr Shenoy’s collaboration allows them to offer advanced surgical techniques and comprehensive care for patients.
Contact Form for Hypospadias Foundation
Please fill all clinical details and upload pictures and clinical summaries (if available)