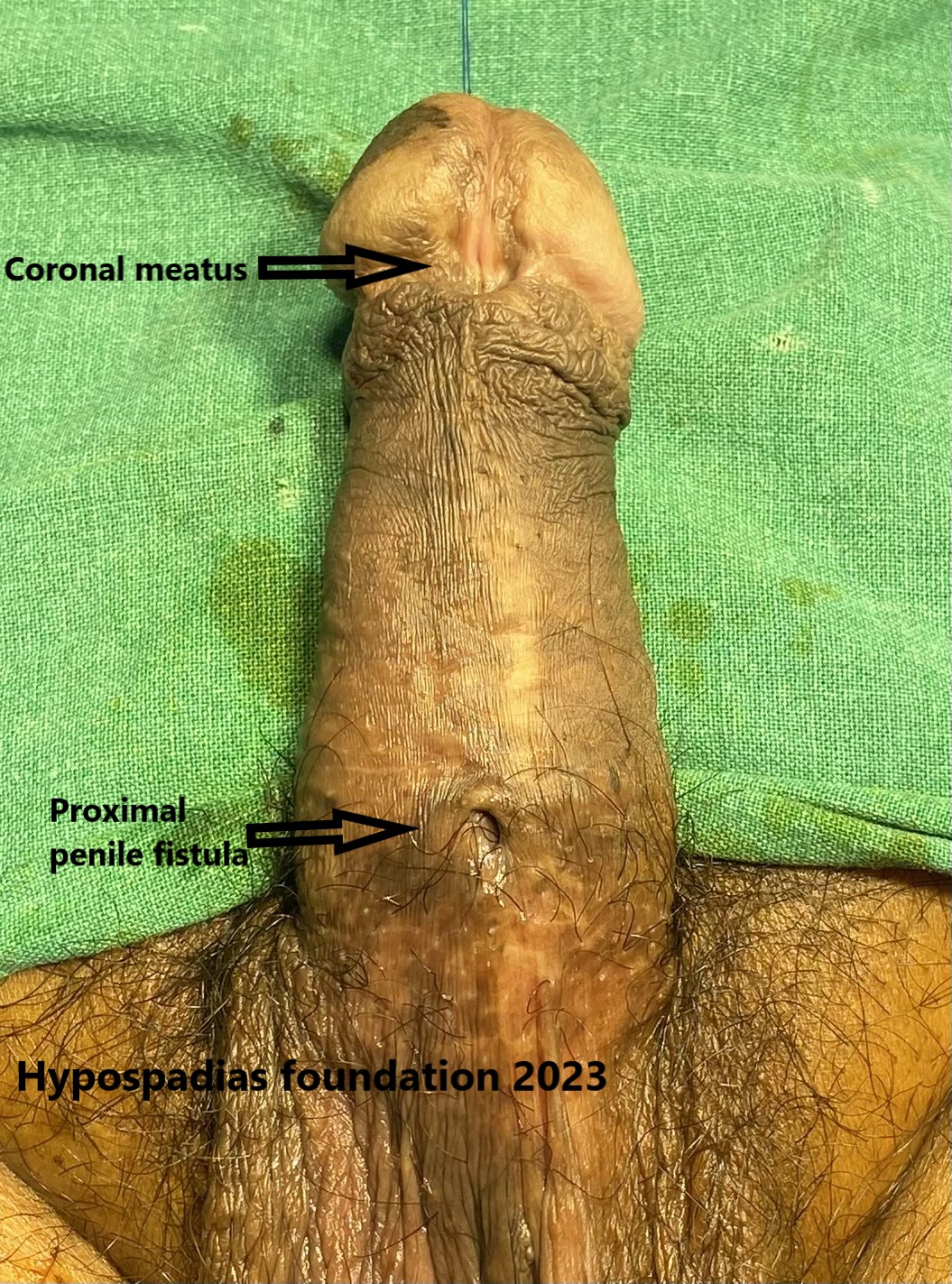
Single stage hypospadias repair in an adult, Mr MP, 25 years male presented with difficulty in retracting foreskin. There was no chordee. He was started on steroid cream massage for 2 weeks for the phimosis. Reassessment after 2 weeks showed that we were able to retract the prepuce partially. Partial retraction of the prepuce showed that the MP had a glanular hypospadias with a megameatus variant. He also had spraying of urine and was very concerned about cosmetic appearance of his penis. He was counselled for surgery for hypospadias along with circumcision.
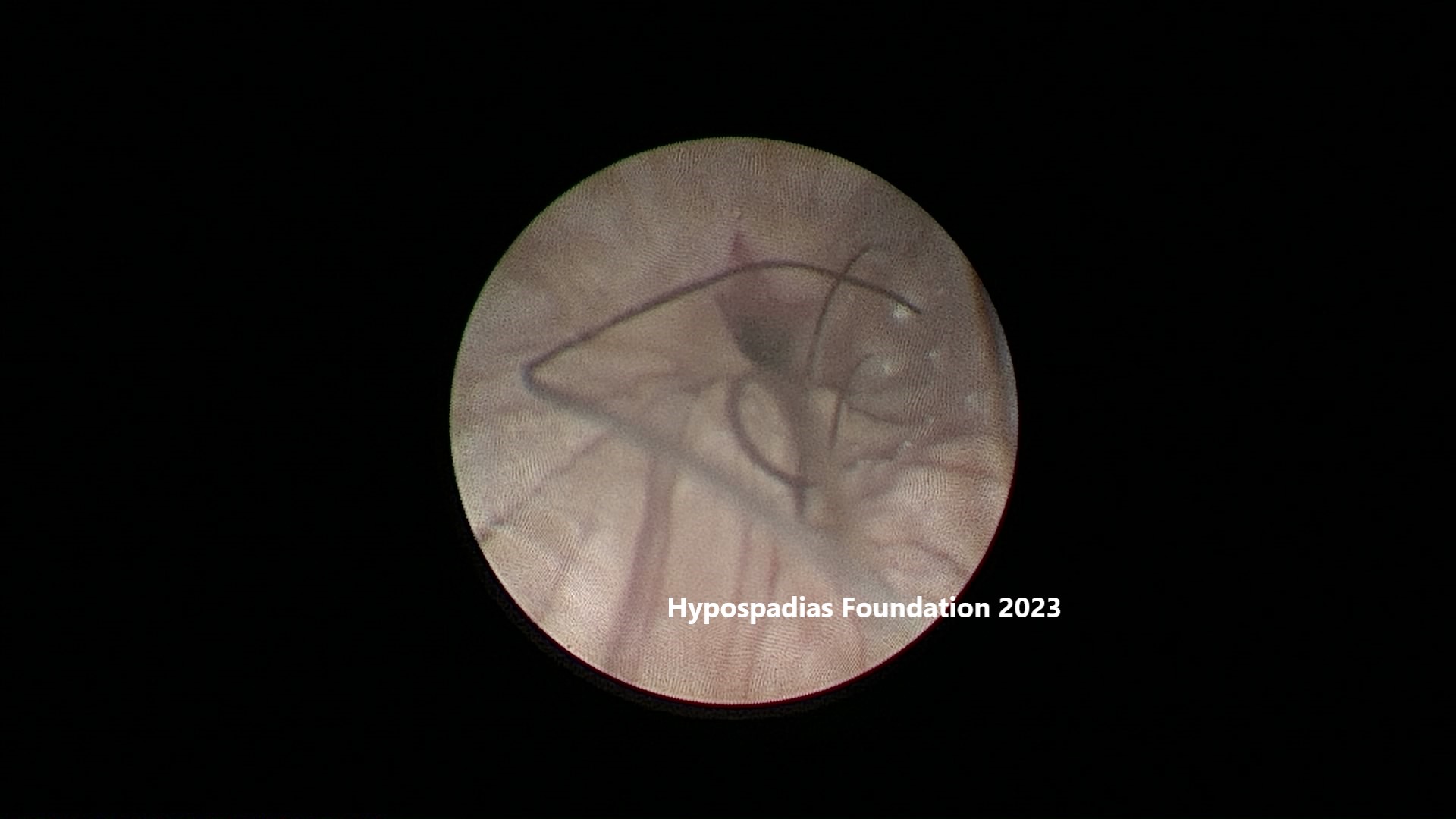
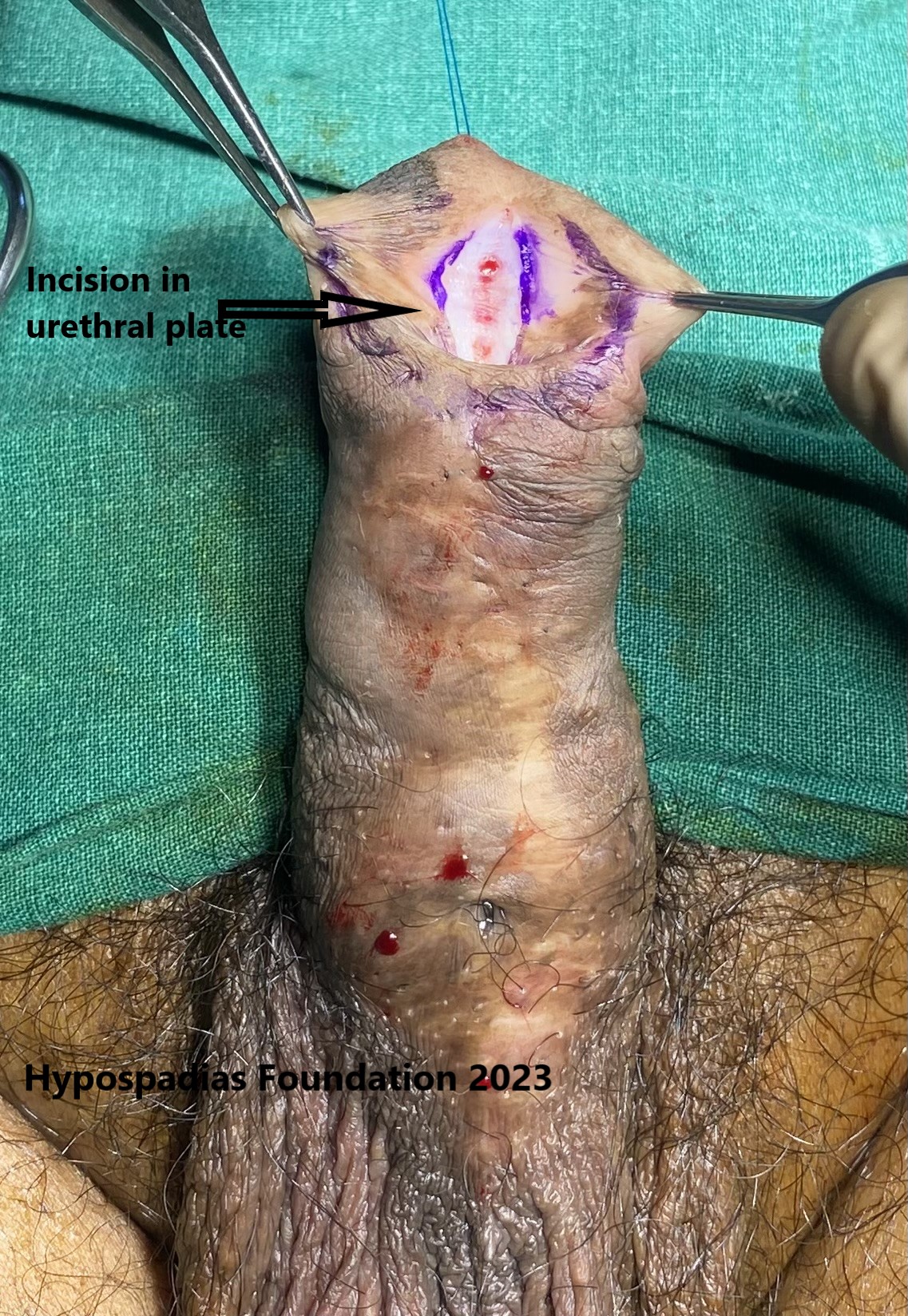
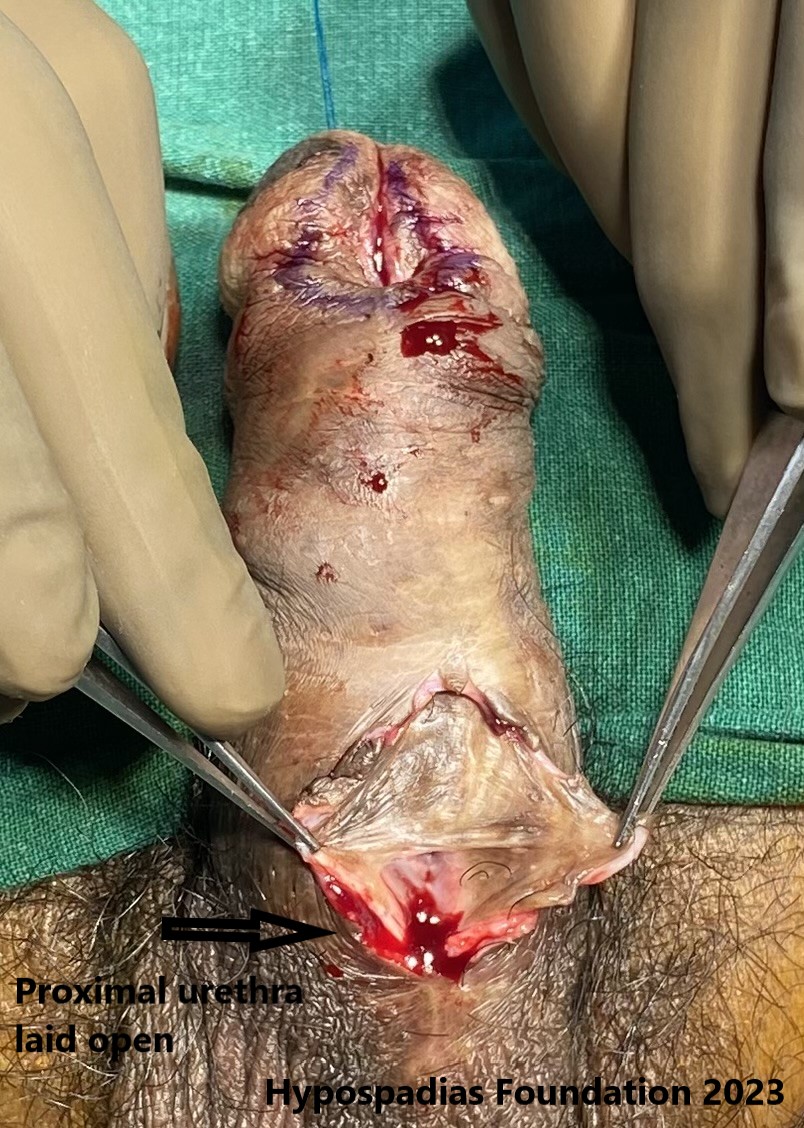
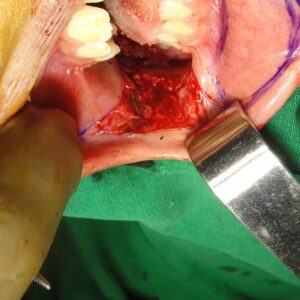
On table examination showed that the patient had a glanular hypospadias with a meatus which was abnormally large, and prepuce was intact. Stay stitch was taken using 4-0 prolene. Circumcoronal marking was done and local anaesthesia with adrenaline was infiltrated at the marked site. Degloving was not done since there was no chordee. Midline incision was given in the dorsal urethral plate and transverse ledge was divided. Glans wings were widely raised and mobilized. Distal urethroplasty was done by continuous sutures using 6-0 PDS over 12 Fr silicone catheter. Local tissues were closed over the urethroplasty using 6-0 PDS. Local dartos flap was raised and sutured over the urethroplasty as a water proofing layer using 6-0 PDS. Glansplasty was done using 5-0 PDS. Glans epithelium was closed using 6-0 PDS. Marked prepucial skin was excised leaving only collar skin and skin was sutured using 6-0 PDS. Sterile dressing was done at end of hypospadias surgery.


Dressing was removed after 7 days and the catheter was removed after 14 days of hypospadias repair. The patient passed urine well and the would healed well with a good cosmetic result. MP was very happy with the overall cosmetic and functional result of hypospadias repair.
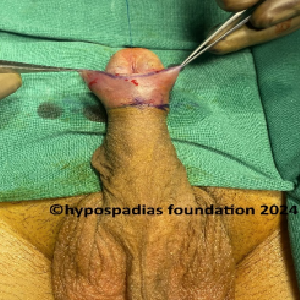

Picture 2a &2b: Marking of the incision.


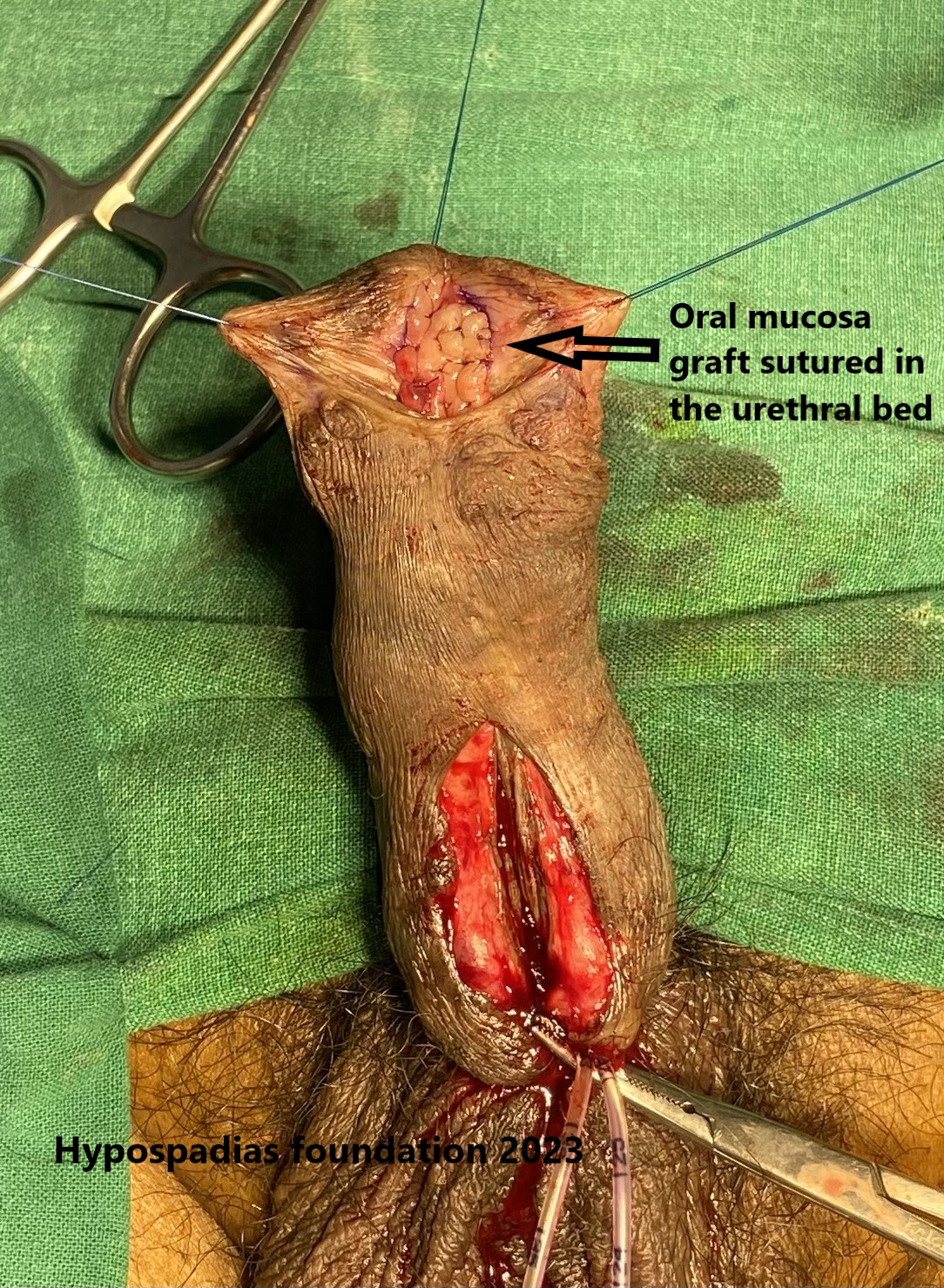
Picture 3a & 3b: Picture showing midline incision in the urethral plate and glans wings mobilization.


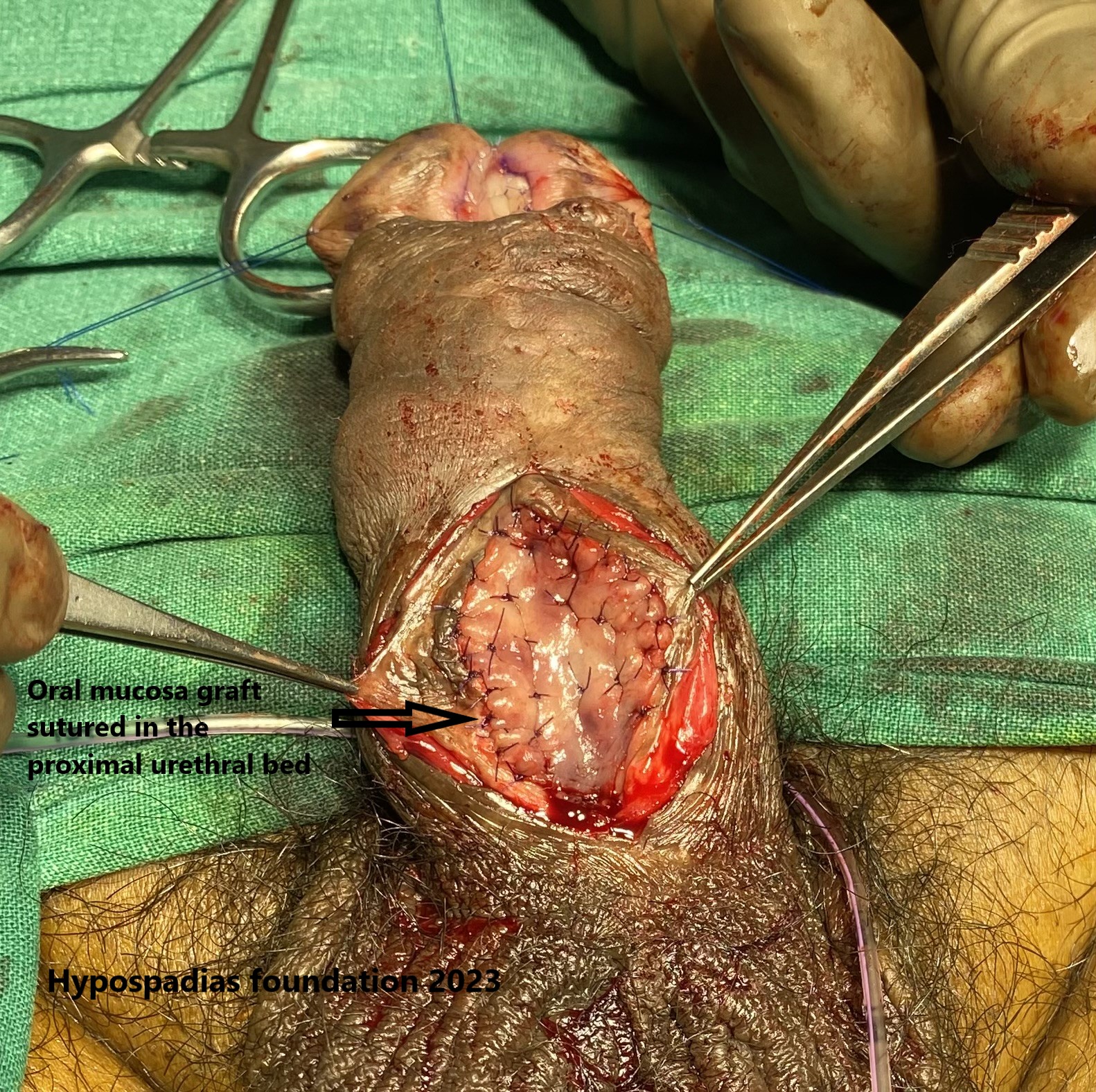
Picture 4a & 4b: Distal urethroplasty done and local flap mobilized to suture over the urethroplasty as a waterproofing layer.


Picture 5a &5b: Completion of repair after surgery and operated site assessment at post operative day 14.


Picture 6a & 6b: Cosmetic result at 4 weeks post-surgery
Picture 7: Post surgery, MP passed urine in good stream
Single stage hypospadias repair in an adult
Hypospadias is a condition in which the urinary opening is on the underside of the penis instead of at the tip. Some of these cases may be missed in childhood. This can happen in:
- Case of mild hypospadias:In mild hypospadias such as present case of glanular hypospadias with MIP variant, the urinary opening may be very close to the tip of the penis. This may not cause any obvious symptoms, and hence may be missed in childhood.
- Presence of complete foreskin:Most of the hypospadias is associated with an incomplete ventral foreskin. Certain types of hypospadias such as glanular hypospadias and MIP variant of hypospadias are known to have complete foreskin. Hence examination of the meatus after retracting the prepuce is necessary in a boy or an adult with suspicion of hypospadias.
- Missed diagnosis:In some cases, diagnosis may be missed if thorough examination is not done in childhood.
Adults need not worry if the diagnosis is missed in childhood. Hypospadias repair can also be done in adulthood successfully. The goals of adult hypospadias repair are as follows:
- Create a functional urethral opening at the tip of the penis.
- To straighten the penis to allow for normal sexual function.
- To improve the cosmetic outcome of the penis
The type of hypospadias surgery depends on the severity of hypospadias, presence of chordee and prior surgical history. An expert hypospadias surgeon will consider all the above factors and take an informed decision and choose the right repair.
About Hypospadias Foundation
Hypospadias Foundation is located at MITR hospital in Kharghar, Navi Mumbai in the state of Maharashtra, India. Every year we get children and adults from all around the country and the world in search of a cure for hypospadias. Our dedication, determination, and perseverance in the field of hypospadias has helped us achieve excellent outcomes.
Dr A K Singal is a top and expert surgeon who has dedicated his life in treating children and adults with hypospadias. His expertise in this area has helped us achieve excellent outcomes in adults and children with hypospadias.
Dr Ashwitha Shenoy is an expert pediatric urologist with special interest in pediatric urology and hypospadias. Both Dr Singal and Dr Shenoy work together to give best results for hypospadias surgery in India for both children and adults.
Contacting the Hypospadias Foundation:
- Email: hypospadiasfoundationindia@gmail.com
- Phone for appointment or Teleconsult with Dr Singal/ Dr Shenoy:
-
- +916262840940
- +916262690790
+919324180553 (whatsapp and teleconsult
Keywords: glanular hypospadias repair, MIP variant of hypospadias, single stage hypospadias repair in an adult, mild hypospadias repair, complete foreskin in hypospadias, missed hypospadias, adult hypospadias repair, hypospadias diagnosis in adult, expert hypospadias surgeon, top hypospadias surgeon, excellent outcome in hypospadias surgery