A 5 years old boy was referred to Hypospadias Foundation after two previous failed surgeries. The child had complications of previous hypospadias surgeries such as distal open area due to dehiscence, distal meatus, chordee (bend of penis) and a thin glans bridge. A 5 years old child failed hypospadias repair.

Notice the distal opening of urethra with a thin glans bridge

After deloving the penis, there is bend at the tip of the penis (chordee)

Chordee correction done by 12 o’clock tunica albuginea plication
As a first step, the penis was degloved and chordee checked. There was still significant bending of the head of the penis (pic 2). Chordee correction: Chordee was corrected by Tunical Albuginea plication at 12 o’clock on the upper side of penis and there was no chordee on rechecking the penis (pic3). An onlay flap was harvested from dorsal penile skin with very good dartos blood supply for urethroplasty (pic4). The flap was rotated around the side of penis and brought to underside of penis for urethroplasty (pic5). The urethroplasty was finished uneventfully but there was severe skin shortage on the underside of penis due to two previous surgeries. Multiple z plasties were done to mobilize and stretch the skin for covering the underside of penis (pic6). A 5 years old child failed hypospadias repair.
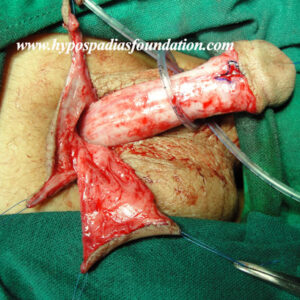
Onlay flap harvested from dorsal penile skin. Notice good blood supply from dartos tissue

Onlay flap ready to for distal urethroplasty after rotating it down to underside of penis

Completed urethroplasty for failed hypospadias. Due to shortage of skin multiple Z plasties were done
Catheter was left in place for ten days for healing. After removal of catheter, the child passed urine in good stream from the tip and is doing very well without any need for further surgery after 6 months of checkup.













