Circumcision is a procedure done to remove the foreskin over the glans. Boys hypospadias circumcision The definite indications for circumcision in a child are recurrent balanoposthitis (foreskin infections), failure of local steroid therapy in phimosis and infant boys with recurrent urinary infection. Another important reason why parents choose circumcision for their child is for religious or cultural reasons.
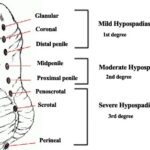
During circumcision it is necessary to retract the foreskin completely and check for the position of the meatus. This is necessary because hypospadias can be sometimes missed and once the foreskin is excised, hypospadias repair becomes challenging. The hypospadias variants which can be missed are glanular hypospadias, MIP (megameatus intact prepuce) variant and chordee without hypospadias. Any surgeon performing the circumcision in a child should be vigilant and circumcision
should be avoided at all costs in children with hypospadias.
The reasons to avoid doing circumcision in children with hypospadias are as follows:
1. Foreskin is required for skin closure in hypospadias: Hypospadias is generally associated with deficient penile ventrally and excess foreskin dorsally. During hypospadias repair if the child has already undergone circumcision, then we may encounter difficulty in skin closure.
2. Dartos flap from foreskin is used in urethroplasty: In any urethroplasty we suture multiple layers of tissues over the urethroplasty to decrease the chance of fistula formation. This includes local tissues and dartos flap. In children who have undergone circumcision, dartos flap is unavailable to cover the urethroplasty.
3. Use of prepuce in urethroplasty: Foreskin may be required for urethroplasty in children with poor urethral plate and shallow glans groove. Prepucial onlay flap urethroplasty is a good choice in these children. This is possible only if the foreskin is available. Hence in children who have undergone circumcision this technique will not be possible.
Circumcision, though a simple procedure, has its specific indications in children. Not all boys with hypospadias need circumcision, and when deemed necessary, it should be approached cautiously. Identifying hypospadias during circumcision requires surgeons with keen observation skills to diagnose the condition accurately. The procedure should be abandoned if there’s any doubt, and the child should be referred to a specialist pediatric urologist for further management.
Do consult a specialist pediatric urologist before planning circumcision for your child if you have doubt or your doctor has told you that there may be hypospadias or chordee.
At Hypospadias foundation, we get children from all over India and from more than 25 countries all over the world in search of cure for hypospadias. At our centre we treat adults and children after multiple previous unsuccessful surgeries. Our experience clearly shows that previous circumcision makes subsequent hypospadias repair surgery difficult.
Fill up contact form: https://www.hypospadiasfoundation.com/contact/
Contact Form for Hypospadias Foundation
Please fill all clinical details and upload pictures and clinical summaries (if available)