48-year male presented to us with complaints of passing urine from scrotal region since childhood. He had undergone three hypospadias surgeries elsewhere in the past but still he had multiple urethral fistulas on the underside of the penis. 8 years ago, he developed acute retention of urine, likely due to a suspected urethral stricture. A suprapubic catheter (SPC) was inserted and since then he was on SPC for urine drainage. He visited multiple centres across India from Delhi to Bangalore to Chennai in hope of cure, but everyone dissuaded him for further surgery. Finally, he visited hypospadias foundation for an opinion.
On examination in the OPD, he was primarily draining urine from the SPC. We could see three urinary openings – one meatus was at the penoscrotal junction, and he also had a scrotal and a mid-penile fistula. On clamping the SPC, we checked his urine stream – the stream was poor with a uroflowmetry flow rate of 2.5ml/second and there was spraying of urine.
A retrograde urethrogram was done which showed narrow distal urethra with diverticulum in the rest of distal urethra upto the membranous part of urethra.
We planned a cystoscopy assessment of the proximal urethra following which he was planned for a staged oral mucosa graft urethroplasty.
Stage 1 Oral Mucosa graft urethroplasty:
Cystoscopy showed urethral diverticulum from the penoscrotal region to the membranous urethra. The distal urethra was found to be strictured – we were not able to pass the cystoscope.
Surgery was started by taking a stay stitch over the glans using 4-0 prolene. Complete degloving was done and chordee was checked- no residual chordee was observed. Urethral diverticulum was laid open till normal urethral mucosa was identified. Unhealthy distal fibrotic strictured urethra was removed completely. Proximal diverticulum site was trimmed and proximal urethroplasty done upto the penoscrotal region with 5-0 PDS over a 14Fr silicone catheter. Distal urethral bed was prepared for placement of oral mucosa graft. Glans wings was widely raised.
Oral mucosa graft was harvested from inside of both the cheeks measuring a total of 11cm X 2cm (6cm and 5cm). Graft was defatted slightly and quilted in place using 5-0 vicryl. Pressure dressing was applied, and the catheter was fixed to glans stitch. Dressing and catheter were removed after 10 days.
Graft uptake was 100% with no graft loss. After 21 days, local steroid massages were started and continued till 5 months.
Stage 2 Oral Mucosa graft Urethroplasty:
Graft was soft and supple at 6 months after graft placement. Surrounding skin was also healthy. At stage 2, graft edges were marked. Local anaesthesia (lignocaine with adrenaline) was infiltrated at the marked site. U shaped incision was given and deepened till the corpora. Urethroplasty was done over a 14Fr silicone catheter with 5-0 Vicryl in 2 layers. Local dartos flaps were used for second layer coverage. Skin was closed in 2 layers and dressing was done. Suprapubic cystostomy was done using 14 Fr malecot’s catheter. Dressing inspection was done on post operative day 4 and every 4th day thereafter. During every dressing change betadine wash was given and re dressing was done. Per urethral catheter was removed on post operative day 14 and suprapubic catheter was removed on post operative day 21. Patient was passing urine in good stream without pain or leak after catheter removal. At his final checkup, 6 months after surgery- the cosmetic result was good, and the patient was passing urine from the glanular meatus in good stream.

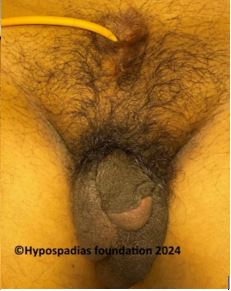
Pic 1: On clinical examination, the meatus was at the penoscrotal region with fistula at mid penile and scrotal region with unhealthy distal skin and SPC in situ


Pic 2: Chordee assessment by artificial erection test and no chordee noted. Stricture noted in the distal urethra.


Pic 3: Proximal urethral diverticulum laid open, trimmed and proximal urethroplasty done


Pic 4: 11cm x 2cm Oral graft harvested from both cheeks and sutured over the urethral bed using 5-0 vicryl


Pic 5: 100% graft uptake and graft noted to be soft 6 months after stage 1, planned for stage 2 repair


Pic 6: Incision given at the margin of the graft and first layer of urethroplasty complete


Pic 7: Local dartos flap sutured over the urethroplasty, Glansplasty done, completion of stage 2 repair
Never give up hope even if multiple hypospadias surgeries have failed
Hypospadias treatment in adults especially if previous surgeries have been unsuccessful, is a difficult task. The complexity of the condition and the potential for complications can often necessitate a staged repair, maybe even in 3 stages. A lot of adults in this century, underwent surgery as children way back in the past and some of them did not get good results even after multiple hypospadias surgeries. With advancing knowledge and expertise, the results of hypospadias repair (urethroplasty) in such cases have improved.
Reasons for multiple surgeries in adults with hypospadias may include:
- Development of complications: The common complications which can occur after hypospadias repair are urethral strictures, fistulas, diverticulum, hairy urethra or residual chordee. These may require additional surgical intervention.
- Unsatisfactory cosmetic results: The patient may be unhappy with the appearance of their penis following the initial surgery.
An adult with multiple failed hypospadias surgeries, generally has no normal hairless penile skin left for hypospadias repair. Hence in such patients, it may be better to use skin from inside the mouth for making the new passage. The skin is taken from inside of cheek or lips and is called oral mucosa. The defect heals very fast and generally without complications. The oral mucosa graft adapts to penile location very well and has great long-term results in redo hypospadias repairs. While some of these cases are suitable for a single stage surgery, some may require two stage surgery depending on the severity of the defect. Nonetheless, Oral Mucosa Graft Urethroplasty remains a great option with best long-term results for children and adults with Failed Hypospadias.
It’s important to note that multiple surgeries can be physically and emotionally demanding. It’s essential to have a strong support system in place and to communicate openly with your hypospadias surgeon about your concerns, experiences and your expectations. If you have undergone multiple hypospadias surgeries, it’s crucial to consult a qualified hypospadias surgeon who can assess your condition and recommend the best treatment plan.
At Hypospadias Foundation in India, Dr Singal and his team offer specialised treatments with best hypospadias surgery results in the world. Children and adults from more than 20 countries such as Dubai & UAE, Bahrain, Iran, Iraq, Afghanistan, Saudi Arabia, Pakistan, Bangladesh, Malaysia, Tanzania, Nigeria, Congo, Ethiopia, Kenya, Nepal, Indonesia, Egypt, Jordan etc come for treatment at our foundation. It is indeed heartening to see them go back with final cure from hypospadias.
Dr A K Singal is regarded as the best hypospadias surgeon in India and in the world for treating children and adults with hypospadias. If you are looking for a highly skilled and experienced pediatric urologist and hypospadias surgeon for yourself or your child, then Dr Singal is an excellent choice.
Dr Ashwitha Shenoy is an expert pediatric surgeon with a special interest in pediatric urology and hypospadias. Dr Singal and Dr Shenoy’s collaboration allows them to offer advanced surgical techniques and comprehensive care for patients.



