Chordee is a condition where the penis is curved downward. Most of the times it is associated with hypospadias but can occur without hypospadias. Chordee correction is very crucial step during hypospadias repair. Without chordee correction, urethroplasty should not be attempted because there will be a stress of the urethral passage and there is high risk of complications after surgery.
Chordee surgery is usually successful in correcting the curvature of the penis completely. However, there is a small chance that chordee can come back after surgery. This is called recurrent chordee.
Risk factors for recurrent chordee:
- Incomplete correction of chordee: When the chordee is severe, it must be corrected completely during chordee correction surgery. If there is any residual chordee after chordee correction surgery, it will only worsen in the future.
- Fibrosis during healing: After chordee correction, fibrosis can occur on the underside of the penis during healing process. Sometimes the fibrosis can improve with steroid massage but if it persists then recurrent chordee correction may be required. This fibrosis can be at the level of skin, tissue under skin or even urethra.
- Due to flaps: Recently we have seen some cases where tunica vaginalis flaps were used for second layer cover during hypospadias surgery at other centres. Somehow the flaps didn’t heal well and they caused chordee to come back. Similar outcomes we have seen when a very tight urethra was made from prepucial flaps or koyanagi repair in first surgery.
Symptoms of recurrent chordee:
The common symptoms which children present with are downward bending of the penis, urine which goes backward and may have occasional pain during erections.
Adults with recurrent chordee may have pain during erection, inability to perform sexual intercourse, painful sexual intercourse and infertility
Treatment for recurrent chordee:
If you think you may have recurrent chordee or your child has recurrent chordee, it is important that you see a doctor right away. You need to visit a hypospadias surgeon or a pediatric urologist who has expertise in the field of hypospadias and chordee correction.
Chordee correction can be done by various methods. First and foremost, the cause for recurrent chordee has to be identified and then appropriate method is used to correct chordee. Chordee correction method differs for children and adults.
- If a child presents with residual chordee due to incomplete chordee correction in the past, then the following methods of chordee correction are used: Complete degloving is done and chordee is assessed, if chordee persists even after degloving then the following methods are adopted. If the chordee is due to short urethra due to flaps or tunica vaginalis flaps, we divide them at this stage.

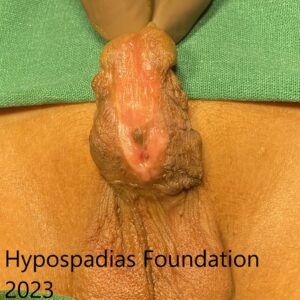
Pre degloving and post degloving chordee assessment
(a) Dorsal tunica Albugenia Plication (TAP): If the chordee is less than 30 degree then it can be easily corrected by placing a non-absorbable suture at the site of maximum curvature on the dorsal side(upper side) of the penis. This will correct the chordee completely.


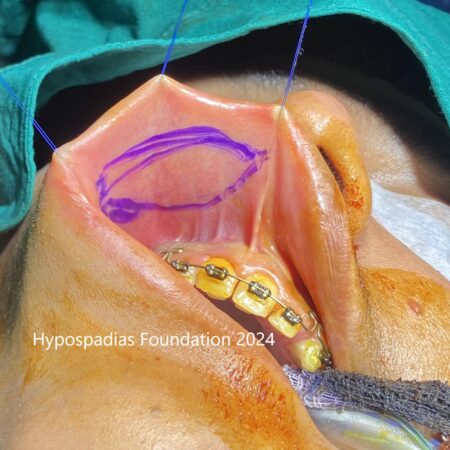
Post Degloving showed less than 30-degree chordee. 12’o clock dorsal tunica albuginea plication done. Chordee completely corrected by this plication.

No chordee noted after 12’o clock dorsal tunica albuginea plication
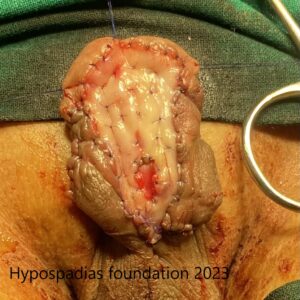
(b) Urethral plate division and Proximal urethral mobilization: If the chordee is more than 30 degrees then one of the reasons for persistent chordee is short urethra, in these cases we will have to divide the urethral plate ventrally and mobilize the proximal urethra. This will effectively correct chordee if it is due to congenital short urethra.


Urethral plate division and proximal urethral mobilization
(c)If chordee persists inspite of urethral plate division then urethral mobilization, ventral corporotomies are done. This will correct the chordee if the cause for chordee is due to disproportionate corporal bodies.

Three ventral corporotomies
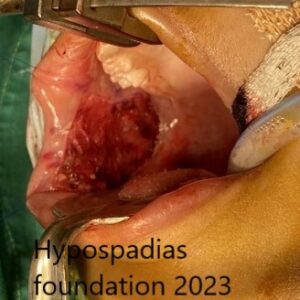
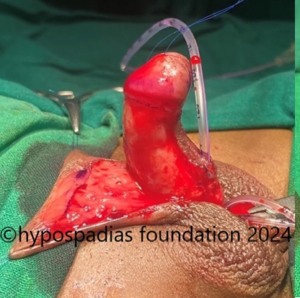
(d) If none of the above measures can correct chordee then we perform a ventral lengthening procedure called as the dermal graft. Deep incision is given in the tunica on the ventral side at the site of maximum curvature and dermal graft is placed at the site. This method is adopted in cases of severe chordee.
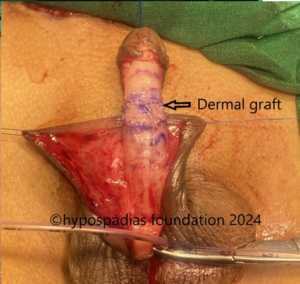
Dermal graft
The chordee is corrected completely after the above steps of chordee correction.
2. If the child presents with severe chordee inspite of complete chordee correction in the past, then it is most likely due to ventral fibrosis. In these cases, along with some or all the above methods, removal of fibrotic tissues from the underside of the penis is important to correct the chordee.
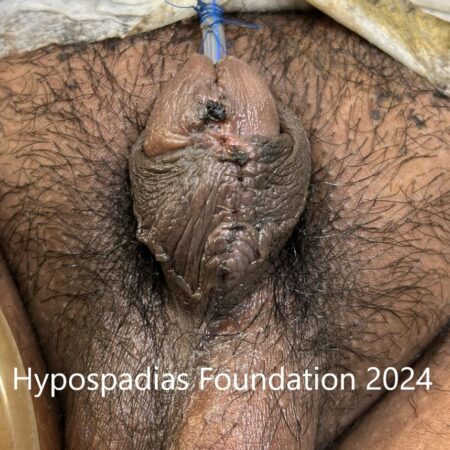
Adults with recurrent chordee after previous surgery
In most of the adults at first we assess the fibrosis and degloving is done. If the chordee is still there, then we divide the urethral plate and mobilise it. Post this, if the chordee still persists, we can correct chordee completely by a method called as “16 dot plication”. In this method, 4 sutures are placed on either side of maximum curvature on the dorsal side, which will correct the chordee uniformly in an adult penis.
In most of the cases of recurrent chordee in addition to chordee correction, urethroplasty will also be required. In redo cases, chordee correction and urethroplasty will most likely be done in two to three stages and oral mucosa graft will be used in more than 95% of such cases. Only in few exceptional we may be able to repair everything in single stage.
About Hypospadias Foundation India:
Hypospadias Foundation in Navi Mumbai, India is dedicated to offering care and cure for chordee and hypospadias in children and adults. Set up in 2008, more than 3000 children and adults have benefitted from care and achieved best in class results for chordee and hypospadias. Dr A.K.Singal and Dr Ashwitha Shenoy, hypospadias expert surgeons at Hypospadias foundation have dedicated their lives to the art and science of hypospadias repair.
If you feel your child or you are suffering from recurrent chordee even after previous chordee correction, then do get it checked by an expert pediatric urologist or a hypospadias surgeon. Chordee correction surgery has good result when done in childhood than in adulthood. Do not hesitate to write to us or contact us
Contacting the Hypospadias Foundation:
- Website: https://www.hypospadiasfoundation.com/
- Email: hypospadiasfoundationindia@gmail.com
- Phone:
- +916262840940
- +916262690790
- +919324180553(whatsapp and teleconsult)
Fill up contact form: https://www.hypospadiasfoundation.com/contact/
Keywords: recurrent chordee, residual chordee, chordee repair, chordee repair surgery, chordee correction surgery, bent penis repair, best hospital for hypospadias in india, best hypospadias surgeon, hypospadias repair in india, adult chordee repair, dermal graft repair, 16 dot plication for chordee
To contact Hypospadias foundation, you can either write to us at hypospadiasfoundationindia@gmail.com or fill up this contact Form
Contact Hypospadias Foundation
Watch Videos of Hypospadias Repair surgery procedure by Dr A.K.Singal, Specialist Hypospadias Surgeon
Contact Form for Hypospadias Foundation
Please fill all clinical details and upload pictures and clinical summaries (if available)