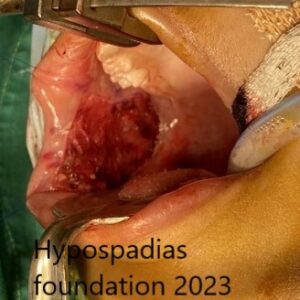
“Mast SP, a 15-year-old male from South Africa, is a case of failed hypospadias repair, having undergone four unsuccessful surgeries elsewhere in the past. Despite previous attempts, the desired result of hypospadias repair was not achieved. He presented to us with complaints of spraying of urine with residual chordee. On clinical examination, we found that the meatus was located at the coronal region. The penis was small with flat glans. He was planned for cystoscopy to assess the status of the native urethra, and redo hypospadias surgery was planned in a single stage or in two stages depending on the cystoscopy findings, addressing the challenges of hypospadias repair in a boy

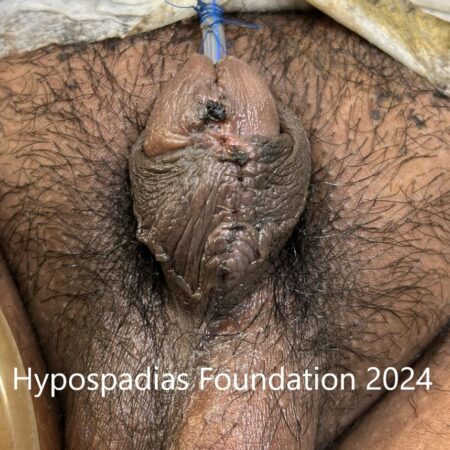
1. Clinical picture showing coronal meatus.
Cystoscopy showed normal urethra. Since the majority of the urethra was normal, we planned for single stage repair, focusing on hypospadias repair in a boy. We chose to proceed with single stage distal oral mucosa inlay graft urethroplasty.
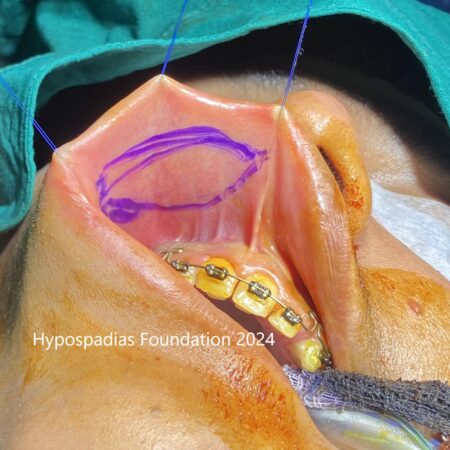
Chordee assessment was done at the start of surgery, and the patient did not have chordee, hence degloving was not done. A midline incision was given in the urethral plate to assess the quality of the urethral plate. There was no scarring in the urethral plate. Since the urethral bed was healthy, we planned to place an oral mucosa inlay graft and perform single stage urethroplasty.


2 a & b. Clinical picture showing the marking of the incision and chordee assessment.
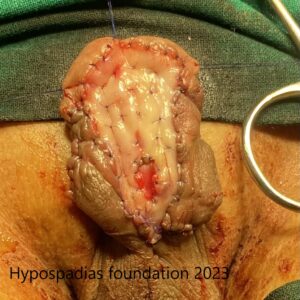
Oral mucosa graft was harvested from the upper lip to perform hypospadias repair in a boy. The graft was defatted and sutured at the urethral bed using 5-0 vicryl. The graft was sutured at the edges of the urethral plate and was quilted in place using 5-0 vicryl sutures. Following inlay graft placement, glans wings were widely mobilized. Urethroplasty was done using 5-0 vicryl stitch, first layer was continuous subcuticular inverting sutures. Second layer was closed using local tissues. Local flap was harvested from the left side and sutured over the urethroplasty as a waterproofing layer using 5-0 vicryl. Glans wings were widely mobilized and distal urethroplasty along with glansplasty was done using 5-0 vicryl.

3 a & b Picture showing site of oral mucosa graft harvest i.e upper lip and oral mucosa graft, it has been placed and quilted in the urethral bed.


4 a & b: Distal urethroplasty completed and local flap harvested from the left side.


5 a & b: Local flap sutured over the urethroplasty, and second picture shows completion of the entire repair.
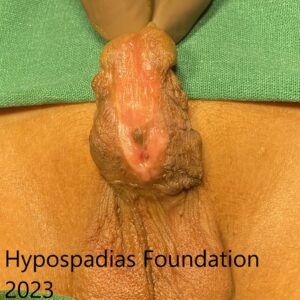
After undergoing hypospadias repair in a boy, the patient had a per urethral catheter and suprapubic cystostomy (SPC). Dressing change was done on postoperative day 4 followed by operated site inspection on every 4th day. Per urethral catheter was removed on postoperative day 21 and SPC was removed on postoperative day 22.

6. Picture showing status at post operative day 15 and second picture shows urine stream after catheter removal.
Post catheter removal, he was passing urine in single straight stream with no leak. Patient was started on meatal dilatation using meatal dilator with mild steroid ointment for 3 months.
Testimonial from the boy’s father in his own words:
We are from South Africa. We got reference of Dr. Singal from a website, post which I got an appointment. Post which they did a proper evaluation and told that he had to undergo a redo hypospadias repair. Based on the evaluation, he had to do redo surgery for hypospadias repair in a boy. We came here on 22nd of December, procedure was properly explained to us. The surgery went well, post care after the surgery was also extremely good. Total support staff, hospital staff took care of my son very well. After the surgery, the discharge process was very fine, post care after discharge was also very good. The steps were properly explained. Today we are finishing the treatment and going out of India to South Africa. From my experience, the overall procedure was very good and extremely satisfying.
Single Stage Hypospadias Repair In A Boy After Multiple Failed Hypospadias Surgeries
Failed hypospadias repair refers to a situation where the initial surgery to correct hypospadias was not successful. Inspite of the best efforts by the surgeon the complications may happen because every healing of every hypospadias patient is different. We do not know the exact reason for complications after hypospadias surgery but here are some factors which may contribute to post-surgery complications:
- Severity of hypospadias: Severe hypospadias repair is more complex and more challenging than mild hypospadias. Total healing time in hypospadias is 3- 4 weeks and it is longer in severe hypospadias. To minimize the risk of complications in severe hypospadias repair, the entire repair may have to be done in 2-3 stages.
- Surgical technique: Different surgical techniques have varying success rates, and the choice of technique can impact the outcome. The choice of technique depends on the type of hypospadias, degree of chordee, glans diameter etc. An expert hypospadias surgeon will choose the best technique after considering all the factors because no two techniques are the same, and no two hypospadias are the same.
- Experience of the surgeon: The experience of a surgeon is an important factor for successful hypospadias surgery. Centre performing more than 50 surgeries per year will have lesser complications compared to the other centres.
- Wound healing: Wound healing is an important deciding factor in complications after any surgery. In hypospadias, wound healing is very slow in adults as compared to children. This may be because of decreased cell turnover with age, a weakened immune system, and reduced blood flow. And if they have any preexisting co-morbid illnesses then healing is slower, with a higher risk of complications.
- Age at surgery: The best age to undergo hypospadias surgery is between 6 and 18 months of age. If not done at this age, it should ideally be done by 5 years of age. Parents are sometimes unable to get the surgery done within 5 years of age, and these children, when they reach adulthood, realize that they need surgery to correct the hypospadias. Outcomes in later age are little inferior to childhood hypospadias surgery but still possible. Adults with hypospadias need not lose hope because it’s better late than never. At Hypospadias Foundation, we have been able to achieve good outcomes with cosmetic result with a success rate of more than 90%, even in adults after multiple previous failed surgeries.
- Underlying medical conditions: Obese or overweight adults, smokers, poor nutritional status, and diabetes are some of the conditions that can lead to slow healing. Overweight patients or diabetics can develop insulin resistance, causing poor healing. Smokers, nutritional deficiencies, etc. can cause decreased blood flow to the operated site, associated with decreased collagen production, which in turn causes slow healing.
Impact and Considerations after failed hypospadias repair:
A failed hypospadias repair can have both physical and emotional consequences for an individual with adult hypospadias and for parents of kids suffering from hypospadias. Complications that can occur after hypospadias repair are:
- Urinary problems: difficulty in urinating, spraying of urine (glans dehiscence), urine passage from multiple holes (fistula), pain in urinating, or urinary tract infections, swelling pf penis during voiding (diverticulum), problems with ejaculation, post void dribbling,
- Residual chordee (curvature): The penis may remain bent, affecting sexual intercourse and, in turn, leading to sexual dysfunction.
- Cosmetic appearance: The meatus may be at a slightly lower level than normal. This may be disturbing for some individuals. In this case, there will be no problems in passing urine, and it is merely the way it looks different from others.
- Psychological impact: As a parent, you may feel helpless and angry after a failed hypospadias. Failure of hypospadias surgery can cause feelings of anxiety, frustration, suicidal tendency, and low self-esteem in an adult. At certain times, adults may need pre- surgery counseling to reduce anxiety and stress. By improving your communication with your doctor and understanding the risks and benefits of surgery, you are more likely to be satisfied with the outcome.
Seeking Help:
If you or someone you know has a failed hypospadias, it’s crucial to seek professional help from a urologist specializing in pediatric urology or hypospadias. They can assess the situation, discuss treatment options, and provide guidance and support throughout the process. Even after previous unsuccessful repairs, there is more than 90% chance that with an expert hypospadias surgeon, the complications can be managed, and your hypospadias can be fully cured.
About Hypospadias Foundation
At Hypospadias Foundation, we get adults and children from all over the world in search of treatment for hypospadias. We provide support and information for children, adults, and their families affected by hypospadias. Dr Singal and Dr Shenoy are deeply devoted to creating awareness and helping patients get the right treatment and best outcomes for hypospadias. Children and adults from more than 25 countries visit Hypospadias Foundation in search of treatment for hypospadias.
Dr A K Singal is a highly experienced surgeon and is regarded as the best hypospadias surgeon in India and in the world for treating children and adults with hypospadias. If you are looking for a highly skilled and experienced pediatric urologist and hypospadias surgeon for yourself or your child, then Dr Singal is an excellent choice.
Dr Ashwitha Shenoy is an expert pediatric surgeon with a special interest in pediatric urology and hypospadias. Dr Singal and Dr Shenoy’s collaboration allows them to offer advanced surgical techniques and comprehensive care for patients.
Contact us:
For appointment kindly contact us at the contact details given below.
MITR hospital & Hypospadias Foundation, Kharghar, Navi Mumbai, India – Tue/Saturday 4:00pm-6:00pm, Call for appointments: +91-9324180553 (whatsapp), +916262840940, +916262690790 Or email us at hypospadiasfoundationindia@gmail.com
Keywords: best hypospadias surgeon India, Best hypospadias surgeon world, complicated hypospadias repair, oral mucosa graft repair, oral mucosa inlay graft, Hypospadias repair in small penis, failed hypospadias repair, oral mucosa graft urethroplasty, results of hypospadias surgery, failed hypospadias surgery, complications of hypospadias, hypospadias surgery, hypospadias surgeon south Africa,
Contact Form for Hypospadias Foundation
Please fill all clinical details and upload pictures and clinical summaries (if available)